While tonsillectomy was almost routine 30-40 years ago, new guidelines limit the criteria for such surgery.
While tonsillectomy was almost routine 30-40 years ago, new guidelines limit the criteria for such surgery.
By Sue Hubbard, M.D.
www.kidsdr.com
If there’s one thing I know after looking down thousands of throats during my pediatric career, tonsils come in many shapes and sizes.
Tonsillar tissue is considered a “secondary lymphoid organ” and is most active in children between the ages of 4 and10. As youngsters go through puberty, the tonsils begin to shrink. As I like to say, “some things get bigger, while tonsils get smaller,” and by adulthood, the tonsils are so small that they can be difficult to see.
The most common complaint about tonsils relates to sore throats and pain with swallowing. While many parents say their child was diagnosed with “tonsillitis,” that doesn’t really tell you what caused the inflammation of the tonsils.
Respiratory viruses are one of the most common causes of viral tonsillitis (and there are tons of those), with Group A strep being the most common cause of bacterial tonsillitis. Mononucleosis caused by Epstein Barr virus also causes a painful tonsillitis and is often seen among teens (this is why mono is called the kissing disease), although mono is not exclusive to the teen group.
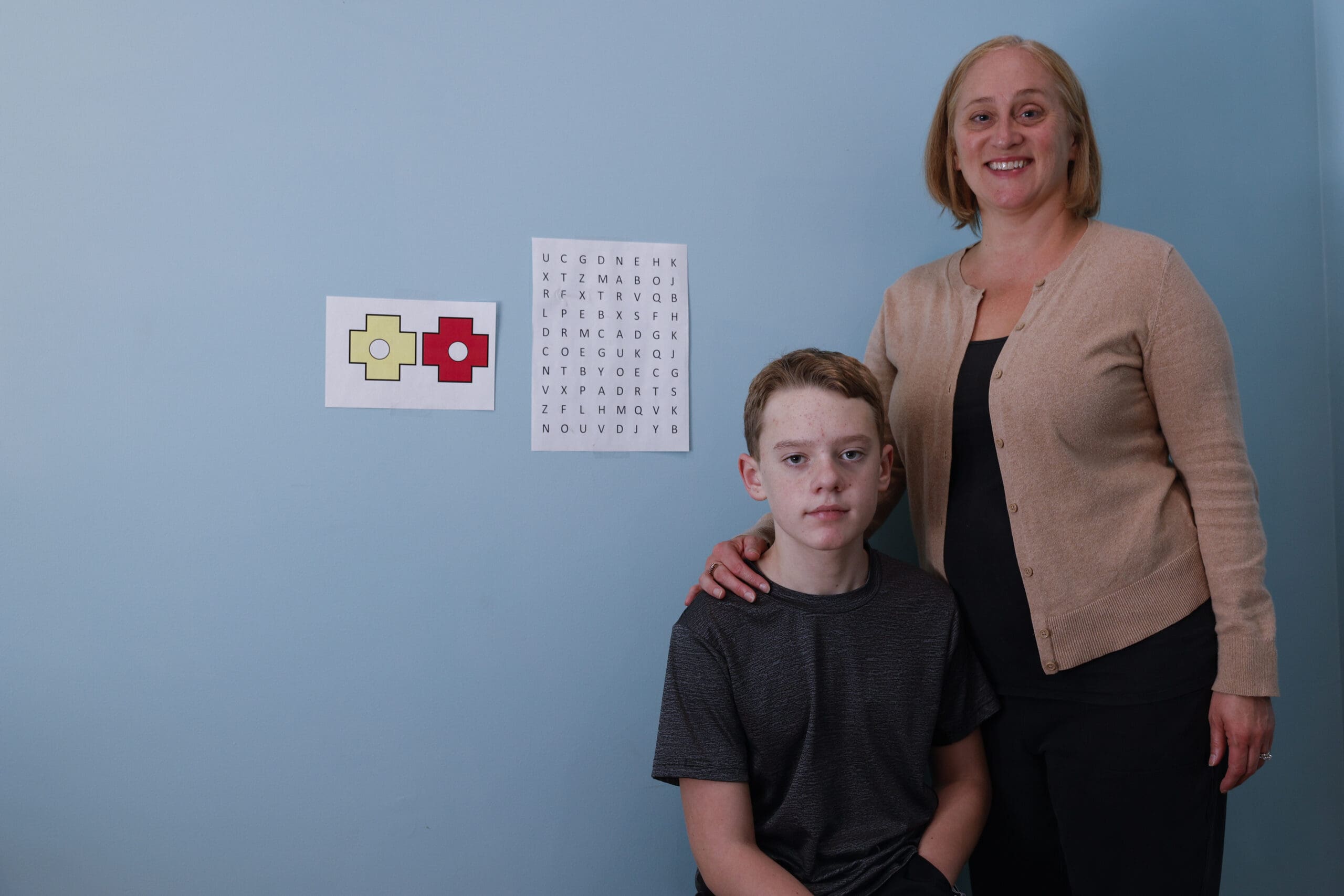
Recurrent “tonsillitis” associated with painful sore throats and large tonsils is often the reason parents ask about a tonsillectomy for their child. While tonsillectomy was almost routine 30-40 years ago, the recommendations for tonsillectomy have continued to change since the 1970s. Even so, over a half a million tonsillectomies are performed each year in the United States.
The newest guidelines, published in January by the American Academy of Otolaryngology, provide updated recommendations as to when tonsillectomy might be recommended. These guidelines state that children should have at least seven episodes of throat infections in a year (both viral and/or bacterial) or at least five episodes each year for two years, or three episodes annually for three years before they become candidates for surgery. All of these infections should be documented by a physician.
The expert physicians who drew up the new guidelines stress that “children who have fewer episodes really aren’t going to see a lot of benefit” and the new recommendations help to minimize the risks (infection and bleeding) and pain of the surgery in children.
As with many things in medicine, things change, hopefully always to improve the outcome for the patient. The new recommendations also included guidelines on tonsillectomy for sleep-disordered breathing.
Dr. Sue Hubbard is a nationally known pediatrician and co-host of “The Kid’s Doctor” radio show. Submit questions at www.kidsdr.com.
(C) 2011, KIDSDR.COM
DISTRIBUTED BY TRIBUNE MEDIA SERVICES, INC.
May 22, 2011 – June 4, 2011 Edition